Pelvic Organ Prolapse – What is it? How does it happen? How do I know if I have it? How it is treated?
Pelvic Organ Prolapse (POP) occurs when one or more of the pelvic organs descend from its normal anatomical position from within the pelvic girdle. This can most commonly include the bladder, the urethra, the uterus or the rectum.
There are many types of prolapse, and these will have various names depending on the organ or organs that have descended or alternatively where the prolapse has occurred within the pelvic cavity.

The severity of the prolapse (how far the organ or organs have descended) will also likely be noted by your health care practitioner; usually on a scale of Grade 0-Grade 4 or stage 0- IV depending on the quantification system used. A prolapse can occur inside the pelvic cavity, or can protrude outside of the vaginal opening. The higher the grade or stage of prolapse, the more the prolapse has descended towards or out of the vaginal opening. The severity of organ descent does not always correlate to symptom severity however. There are those who have minor objective prolapses when assessed by a health care provider but note significant prolapse symptoms, while others with more significant objective descent of the organs may have barely any symptoms at all.
The pelvic floor muscles, as well as the pelvic fascia/connective tissues support the pelvic organs. Repeated pressures from strain (which typically occurs on a relaxed pelvic floor) and valsalva (which is a forced exhalation against a closed glottis, mouth and nose) to these structures can worsen the descent of prolapse. 1
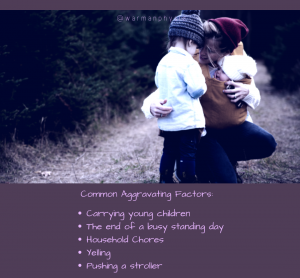
Some activities/conditions that can cause increased strain/valsalva to the pelvic floor and which are risk factors for POP are: vaginal delivery, having a chronic respiratory condition, as well as chronic constipation.2,3,4 Prolapse symptoms can worsen following activities such as heavy or repetitive lifting (like carrying children all day!!) Symptoms are often worse later in the day as the effects of gravity become more noticeable.
The symptoms of POP can vary. Some of these symptoms include heaviness or discomfort in the vagina, difficulty with constipation, difficulty emptying the bladder or bowel completely, urinary or fecal incontinence, difficulty with insertion of tampons, discomfort during sex, and irritation of exposed vaginal tissue.
The literature supports physical therapy and pelvic floor muscle training (PFMT) as an effective way to conservatively manage POP symptoms and severity of organ descent. 5,6 Physical therapy can help by giving clients strategies to help manage their intraabdominal pressure systems during activities that increase pressure and strain to the pelvic organs and pelvic floor such as lifting, carrying, coughing, jumping, sneezing, etc. Often ‘The Knack’ is a technique taught where the client performs a pelvic floor contraction prior to an activity that would cause a significant increase in intraabdominal pressure to help decrease the strain to the pelvic floor. A pelvic floor physical therapist will perform an internal pelvic exam to assess the strength and tone of the pelvic floor as well as grade the prolapse. If there are other issues found during the assessment such as incontinence or pain, those will also be addressed. Education regarding toileting positions and evacuation techniques to decrease strain on the pelvic floor can be discussed. The physical therapist will also work with the client to help progress them back to their functional and fitness goals and how to modify tasks where needed.
For those whose POP symptoms continue to bother them despite doing some PFMT or those wishing to pursue sports where there may be increased pressures placed on the pelvic floor, a pessary may be a good conservative option. A pessary is a device that is placed in the vagina to help provide support and manage prolapse symptoms by preventing or lessening the descent of the pelvic organs. There are many different types of pessary available depending on the type of prolapse. Usually urogynaecologists, gynaecologists and nurse practitioners fit pessaries, however in some provinces pelvic floor physiotherapists are able to fit and follow these clients.
Others whom have more severe symptoms or severity of POP may choose surgery as an option. The type of treatment for prolapse will vary depending on the severity of the symptoms, the grade of prolapse, as well as client preference.
Conservative management and strategies learned with a pelvic health therapist can be helpful even for those that choose surgical management of their prolapse in resolving some of the pressure management issues that lead to POP.

Maja Stroh is a physiotherapist that has a particular interest in pelvic health and perinatal care. She graduated from the U of S MPT program in 2009 and has been working with pelvic health populations since 2013. Maja’s interest in helping her clients and spending quality time with her family has brought her to Warman Physio where she will be providing services in the Saskatoon and Warman locations.
Maja has a particular interest in the assessment and treatment of pelvic organ prolapse and is available in Saskatoon and Warman.
Our team consists of three pelvic health therapists to assist you including Maja, Kendra, & Haylie.
References:
- Tumbarello, J.A., Hsu, Y., Lewicky-Gaupp, C., Rohrer, S., & DeLancey, J.O. (2010). Do repetitive Valsalva maneuvers change maximum prolapse on dynamic MRI?. International Urogynecology Journal, 21 (10), 1247-1251.
- Mant, J., Painter, R., & Vessey, M. (1997). Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. BJOG: An International Journal of Obstetrics & Gynaecology, 104(5), 579-585.
- Whitcomb, E.L., Lukacz, E.S., Lawrence, J.M., Nager, C.W., & Luber, K.M. (2009). Prevalence and degree of bother from pelvic floor disorders in obese women. International Urogynecology Journal, 20 (3), 289.
- Fornell, E.U., Wingren, G., & KjOlhede, P. (2004). Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta obstetrician et gynecologica Scandinavica, 83(4), 383-389.
- Hagen, S., Stark, D. (2011). Conservative prevention and management of pelvic organ prolapse in women (Cochrane review). Cochrane Database of Systematic Reviews, (12), CD003882.
- Li, C., Gong, Y., & Wang, B. (2016). The efficacy of pelvic floor muscle training for pelvic organ prolapse: a systematic review and meta-analysis. International urogynecology journal, 27 (7), 981-992.